When exploring options for a peaceful and fulfilling lifestyle in later years, many may ponder the health concerns that often come with aging. Among these, vascular dementia is a significant condition that affects numerous individuals worldwide. You might wonder, “Is vascular dementia hereditary?” Understanding the genetic components of vascular dementia is crucial, especially when considering the ideal living environment that supports wellness and engagement, such as a retirement community.
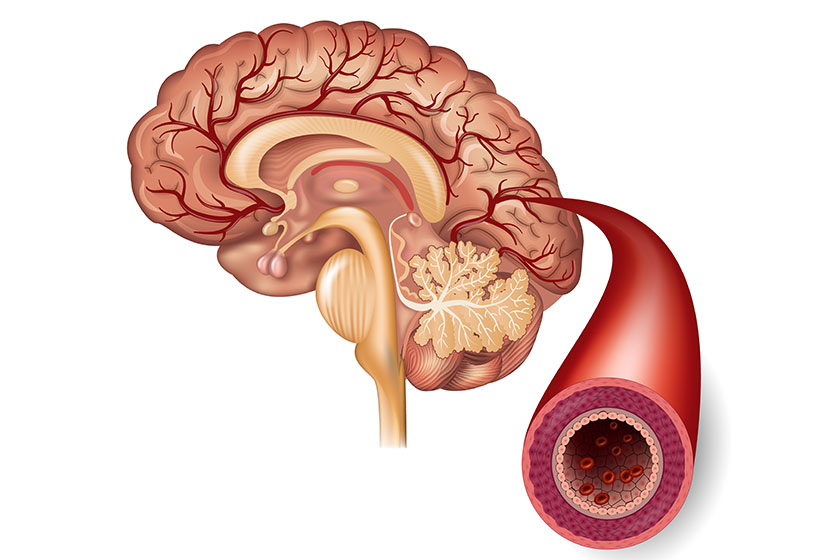
Vascular dementia ranks as the second leading form of dementia, trailing only Alzheimer’s disease and originates from conditions that impede or diminish blood flow to the brain. This reduction in blood flow deprives brain cells of the essential oxygen and nutrients required for their proper operation. Although the primary causes of vascular dementia are more strongly linked to lifestyle and health conditions rather than genetics, there exists a subtle interplay between our genetic makeup and the likelihood of encountering this condition.
The Role of Genetics in Vascular Dementia
It is understood that vascular dementia itself is not directly inherited in the same way some diseases are. Instead, the risk factors for developing vascular dementia, such as high blood pressure, diabetes, heart disease and stroke, can be influenced by genetics.
This means that while you may inherit a predisposition to these conditions, it does not guarantee the development of vascular dementia. The connection between genetics and vascular dementia is complex, involving multiple genes and their interactions with environmental factors.
Lifestyle Over Legacy
Given the genetic predisposition to risk factors, it becomes evident that maintaining a healthy lifestyle is paramount. Engaging in regular physical activity, adhering to a nutritious diet and monitoring health conditions can significantly mitigate the risk of developing the conditions that lead to vascular dementia.
This emphasis on lifestyle is particularly relevant when considering a transition to a retirement community. Such communities often offer senior living amenities and retirement community events that promote a healthy and active lifestyle, indirectly supporting brain health.
A Supportive Environment for Brain Health
When considering the future and the possibility of cognitive decline, the environment in which one chooses to live becomes increasingly important. Retirement communities that offer specialized care, such as Memory Care, can provide a supportive environment that caters to the unique needs of individuals experiencing cognitive challenges.
Genetic Testing and Personalized Care
For individuals apprehensive about their genetic susceptibility to vascular dementia, genetic testing offers valuable insights. Nonetheless, it is imperative to undertake genetic testing with prudence and under the supervision of a healthcare expert. While comprehending one’s genetic predisposition can inform tailored care approaches, it’s essential to recognize the substantial influence of lifestyle choices in mitigating the risk of vascular dementia. Striking a balance between genetic insights and lifestyle modifications is pivotal in developing effective strategies for managing vascular dementia risk and promoting overall brain health.
The Impact of Social Engagement on Cognitive Health
Social interaction holds immense importance in the preservation of cognitive function as individuals progress through the aging process. Active participation in meaningful conversations, involvement in group activities and fostering a sense of community belongingness all serve as potent stimulants for the brain. These interpersonal engagements not only offer enjoyable experiences but also wield profound benefits for cognitive well-being. By promoting mental agility, resilience and overall brain health, sustained social engagement becomes a cornerstone in the pursuit of cognitive vitality across the lifespan.
Technological Innovations in Cognitive Care
Technological innovations have revolutionized cognitive care, offering novel avenues to bolster cognitive health. From brain-training applications to devices aiding daily living for individuals with cognitive decline, these advancements redefine care paradigms. Moreover, these technologies enable personalized healthcare by empowering professionals to closely monitor residents’ well-being and dynamically adjust care plans in real-time. Seamlessly integrating technology into cognitive care enables communities to enhance resident experiences, optimize health outcomes and foster a more holistic approach to cognitive wellness.
Nutrition and Brain Health
A burgeoning body of research underscores the pivotal role of nutrition in maintaining optimal cognitive function. Diets abundant in omega-3 fatty acids, antioxidants and essential vitamins demonstrate a profound correlation with a reduced risk of cognitive decline. By nourishing the brain with these vital nutrients, individuals can potentially safeguard against cognitive impairment and promote long-term brain health. Embracing a diet rich in these beneficial components emerges as a proactive strategy in supporting cognitive vitality and preserving mental acuity throughout life’s journey.
The Role of Physical Activity in Preventing Cognitive Decline
Physical activity stands as a cornerstone in fostering cognitive health, widely acknowledged for its myriad benefits. Through enhanced blood flow to the brain, exercise plays a pivotal role in mitigating the pace of cognitive decline. Residents engaging in such activities are provided with abundant opportunities to uphold their physical well-being, directly influencing their cognitive welfare. Intertwining physical fitness with cognitive maintenance enables individuals to proactively safeguard their mental acuity, promoting a harmonious balance between physical and cognitive vitality.
Environmental Factors and Cognitive Health
The environment one resides in exerts a substantial impact on cognitive health, especially for those susceptible to or grappling with cognitive decline. A safe, stimulating and adaptive environment tailored to residents’ needs profoundly influences their well-being. Secure walking paths, lush gardens and designated areas for relaxation and activities are pivotal features ensuring residents experience a high quality of life. These elements not only support cognitive and physical health but also foster a sense of fulfillment and contentment, creating an environment conducive to maintaining optimal cognitive function and overall vitality.
In answering the question, “Is vascular dementia hereditary?” it becomes clear that while there is a genetic component to the risk factors leading to vascular dementia, the condition itself is not directly inherited. This understanding underscores the importance of lifestyle choices and the environment in managing the risk of vascular dementia.
Retirement communities, with their focus on healthy living, social engagement and specialized care options, offer an ideal environment for supporting brain health and overall well-being in later years. As you consider the next steps for yourself or your loved ones, remember that the power of a supportive and engaging community cannot be overstated in its contribution to a fulfilling lifestyle.